Pharmacist Pioneer Community. Why?
Jul 03 - 2022

It is one of the leading causes of disability in the elderly, as its symptoms begin with severe pain and swelling in the affected joint and soon this pain is accompanied by sensitivity to any slight pressure, difficulty and loss of flexibility in movement, and it may progress to immobility because of pain and its complications, which leads to atrophy in the affected area and loss of its function, especially as it is a progressive disease that worsens without proper treatment.
What leads to osteoarthritis? Are there any preventive methods that protect against its progression?
This is the topic of today's article to answer all of the following questions:
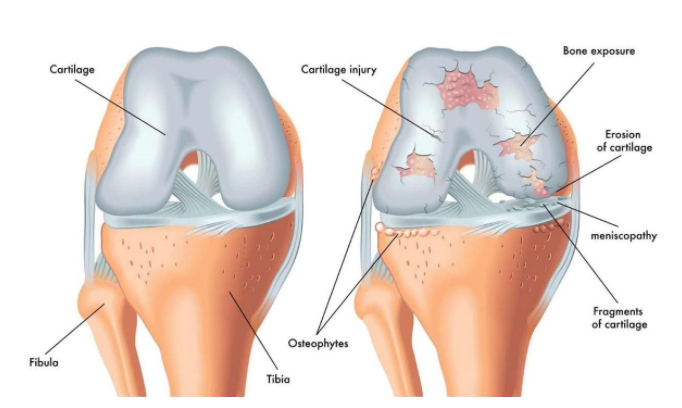
Normally, the joint (the place where the bones of the body meet) is covered with a smooth cartilage layer that helps the bones to move freely against each other and work to protect them by preventing friction, but when the joint is exposed to inflammation and roughness for reasons we will mention later, these cartilages begin to weaken and wear out, leaving the joint without an encapsulating layer to protect and support it, which results in frequent friction between the bones, causing severe pain with every movement.
In response to the cartilage damage, all tissues within the joint become more active than usual as the body tries to repair this damage, but the repair processes may change the joint structure affecting its function and resulting in difficulty moving naturally.
Pain and swelling in the affected area are common symptoms in most bone diseases, that is why the diagnostic methods should complement each other to detect and distinguish osteoarthritis from the rest of the diseases, and these methods are:
By knowing the patient’s experience and through the other diagnostic methods, the doctor diagnoses osteoarthritis by excluding other bone diseases that have laboratory signs and results that distinguish them, and then begins the treatment process by choosing the appropriate treatment for each case according to the rate of disease progression.
All treatment methods do not completely cure it, but only reduce pain and prevent the deterioration of the condition, allowing the patient to practice his life closer to a normal one.
Lubricants: Hyaluronic acid injections provide pain relief by providing some softening and cushioning of the joint.
Vorek Cream, recommended by doctors for its dual effectiveness in relieving joint pain and treating inflammation. It contains 11 active ingredients that play a powerful and effective role in treating osteoarthritis, as it is manufactured with the latest pharmaceutical technologies that guarantee a fast and extended effect throughout the day.
The elderly are most vulnerable, especially those over the age of 50, but all age groups are also vulnerable if some other risk factors are present, and risk factors include the following:
*This article was written by an integrated medical team affiliated with Devart Lab, the leading company in the field of Nutraceuticals in Egypt and the Middle East (Nutrigenomics and Food Fortification), by providing nutrients that are fortified with minerals and vitamins that the body needs on a daily basis to obtain effective results in the least possible time. By using the latest pharmaceutical technologies that ensure full absorption without any side effects.

Jul 03 - 2022

Jun 22 - 2022

Jun 12 - 2022

Jun 05 - 2022